How Long Can Transplanted Hair Last
(Source of Picture) Donor supply is the ultimate limiting factor in hair transplantation for male pattern baldness (MPB) patients. According to Norwood's Classification, a man with advance Class VII balding would still have a rim of hairs at the sides and back of the head. This is labelled as the "Safe Donor Area" that is expected to be permanently covered with hair for a lifetime and therefore, provide permanent coverage when transplanted to the recipient area.
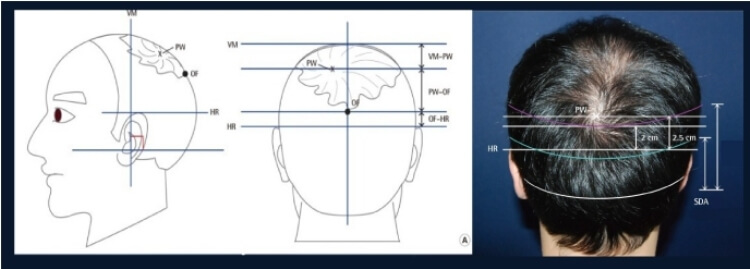
Defining the Safe Donor Zone
The boundaries generally extend from in front of the ears, around the temples, and to the back of the head. Exact mapping of this permanent donor area is still not possible. A rule of thumb is to forecast the maximum extent of alopecia progression). This may help to limit and confine the donor area. In young patients hair loss is progressive and unpredictable. Hair at the temples may recede back toward the ear, while balding area of the crown may dip quite low into the back of the head. A more conservative approach should therefore be adopted in defining the Safe Donor Zone. The most crucial of the safe donor area is the superior border. It was estimated to be about 5.5 to 6 cm from crown whorl (1). Hairs above this border are not recommended for transplant.
Donor Selection in FUE and ARTAS
Hair transplant surgeons have been trying to transplant the maximum-possible number of hair grafts in a single session to cover more of the recipient area. Many surgeons have frequently been in dispute about the appropriate standards for defining a safe donor area. FUE and ARTAS are known to require a much larger donor area when compared to Strip/FUT. It has been a great concern that some hair transplant surgeon chose to ignore this Safe Donor Zone when desperate for the number of grafts. This obviously viloates the true purpose of hair transplant.
Reference
1. J.H.Pak, et al. Predicting the Permanent Safe Donor Area for Hair Transplantation in Koreans with Male Pattern Baldness according to the Position of the Parietal Whorl. Arch Plast Surg. 2014 May; 41(3): 277–284.
